
Performance Categories: To assign hospitals to performance categories, the hospital's interval estimate is compared to the U.S. In addition, the rates reported are "smoothed" to reflect the fact that measures for small hospitals are measured less accurately (i.e., are less reliable) than for larger hospitals. Risk Adjustment: The measures reported are risk adjusted to account for differences in hospital patients' characteristics. If the RAMR is significantly higher than the statewide mortality rate, the provider has a significantly worse performance than the state as a whole. If the RAMR is significantly lower than the statewide mortality rate, the provider has a significantly better performance than the state as a whole. Thus, the RAMR has, to the extent possible, ironed out differences among providers in patient severity of illness, since it arrives at a mortality rate for each provider for an identical group of patients. Performance Categories: The risk-adjusted mortality rate (RAMR) represents the best estimate (based on the associated statistical model) of what the provider’s mortality rate would have been if the provider had a mix of patients identical to the statewide mix. Mortality rate is based on deaths occurring during the same hospital stay in which a patient underwent cardiac surgery and on deaths that occur after discharge but within 30 days of surgery. These activities are very helpful in ensuring consistent interpretation of data elements across hospitals. Data are verified through review of unusual reporting frequencies, cross-matching of cardiac surgery data with other Department of Health databases, and a review of medical records for a selected sample of cases. Along with information about the procedure, physician, and the patient’s status at discharge, these data are entered into a computer and sent to the Department of Health for analysis.

Approximately 40 of these characteristics (called risk factors) are collected for each patient. Cardiac surgery departments collect data concerning patients’ demographic and clinical characteristics. Risk Adjustment: As part of the risk-adjustment process, NYS hospitals where cardiac surgery is performed provide information to the Department of Health for each patient undergoing that procedure. The lowest possible score is 0%, and the highest possible score is 100%. Measure Steward: New York State Department of Healthĭata Presentation: Percentage. If the entire 95% interval estimate is below the national rate for that measure, then the hospital is performing "Significantly Better than the National Rate." If the entire 95% interval estimate is above the national rate for that measure, its performance is "Significantly Worse than the National Rate." Hospitals with fewer than 25 eligible cases are placed into a separate category that indicates that the hospital did not have enough cases to reliably tell how well the hospital is performing. If the 95% interval estimate includes the national observed rate for that measure, the hospital's performance is in the "No Significant Difference" category. Risk Adjustment: The measures of serious complications reported are risk adjusted to account for differences in hospital patients' characteristics. If the ratio is less than 1.0, then the implication is that the provider performed better than the reference population. If the ratio is greater than 1.0, then the implication is that the provider performed worse than the reference population for that particular indicator. Measure Steward: Agency for Healthcare Research and Qualityĭata Presentation: Ratio.
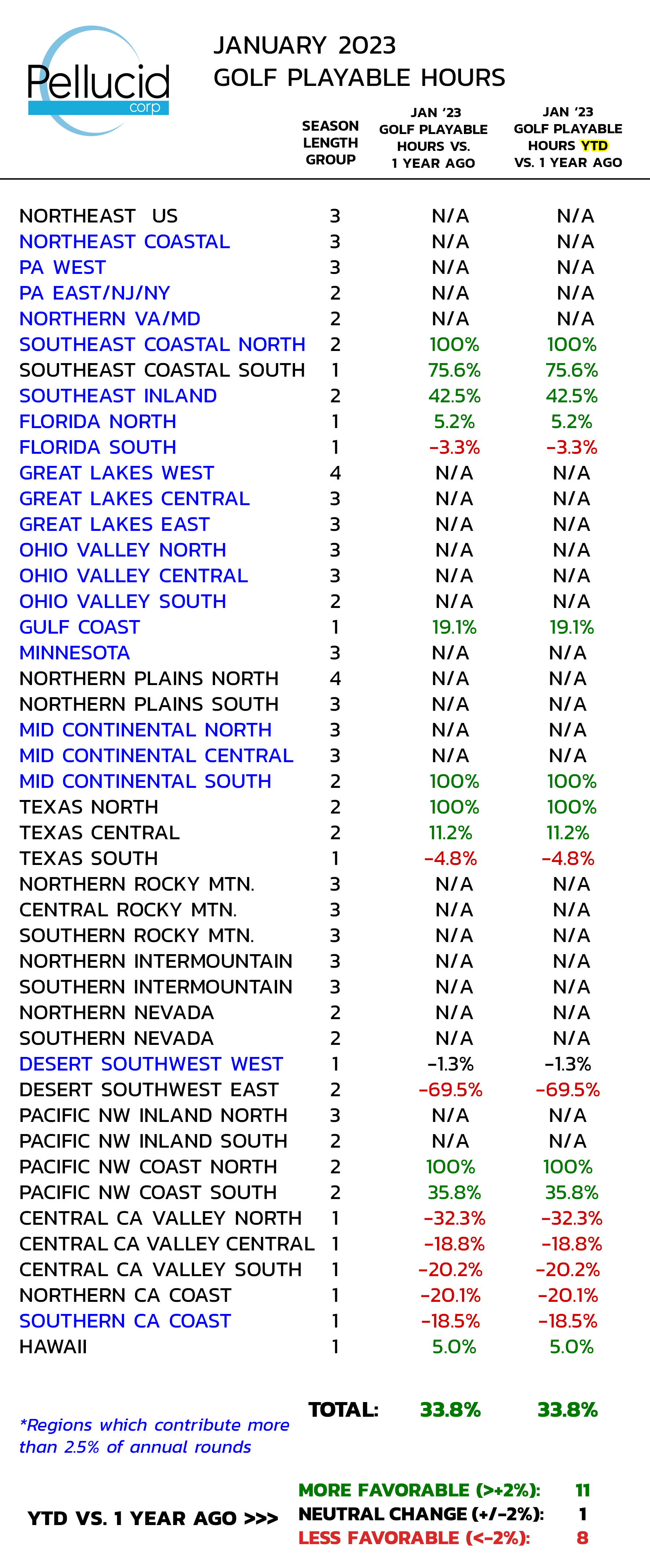
#Pellucid data update#
Generally, this page covers data generated for hospitals by the CMS Quarterly Update Complications of Care This page describes the Methodology used to create values and benchmarks for the different measure types.


 0 kommentar(er)
0 kommentar(er)
